Definition: Syphilitic stromal keratitis is a form of chronic stromal keratitis with vascularization. The term interstitial keratitis was coined in the 1800’s by Hutchinson for congenital syphilis and unfortunately (from the pathologists perspective) is still used.
Incidence/Prevalence: Syphilitic stromal keratitis is the most common manifestation of untreated late congenital syphilis; it occurs in about 20-50% of patients. The prevalence of syphilis is about 10-50 early cases per 100,000 in the U.S. population. At least 12 million cases of syphilis have been reported in adults annually in the world with estimates between 500,000- 1 million affected pregnancies. It has been estimated that about 40% of cases of untreated congenital syphilis will get syphilitic stromal keratitis.
Etiology: Transplacental infection of the fetus is produced by the spirochete, Treponema palladium. The late onset of congenital syphilitic keratitis is thought to be explained by an immune response to microbes or their antigens. Organisms have been identified in the aqueous of patients with congenital syphilis. [Ref 1&2]
Clinical Findings: The initial presentation of congenital syphilis (late untreated) has its onset between ages 5 and 20 as an acute stromal keratitis and iridocyclitis. 80% of cases are bilateral although the initial presentation involves first one eye followed in weeks to months by the fellow eye. Clinically, there are deep stromal chronic infiltrates and edema that may produce several patterns. Multifocal, sectoral, peripheral, punctate, linear, ring and deep infiltrates are all described. Vessels grow in toward the central deep cornea from the periphery. Scrolls of Descemet’s membrane produce the “glasleitern” which has a distinctive web-like clinical pattern.
 Histopathology:
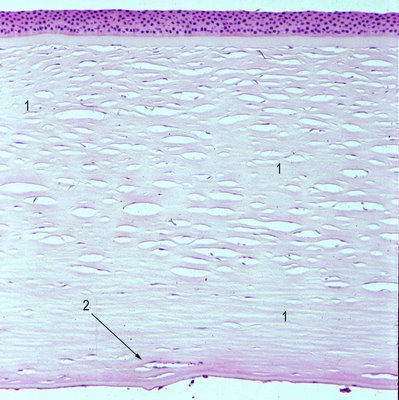
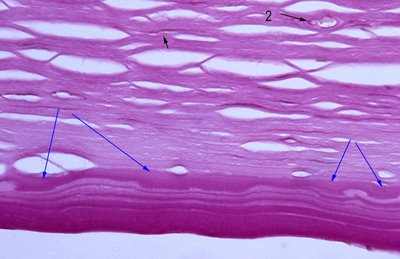
Histopathology: The corneal stroma shows scarring at variable depths (numbers 1), deep stromal vascularization (arrow 2) and during the active phase intense lymphocytic inflammation. The histopathologic findings are frequently termed interstitial keratitis; the findings are similar to a scar after infection and are not specific for syphilis.
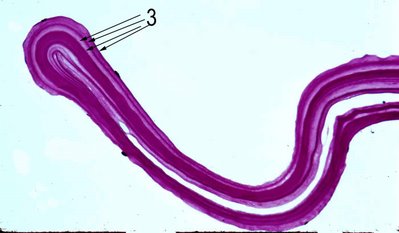
However, about 88% of specimens may show a multi-lamellar intact Descemet’s membrane [Ref 3]. In the figure Descemet's membrane is folded and multilaminar (arrow 3).
Scrolling of Descemet's membrane may also be seen. Secondary guttata are quite common (blue arrows ) but not specific .
 Treatment:
Treatment: Penicillin and topical steroids may shorten the course of disease according to some authors while others suggest that the infants must be treated by 3 months of age in congenital syphilis to prevent the onset of keratitis.
Prognosis: Resolution occurs spontaneously after weeks to months. About 75% of patients will recover vision but if left untreated, stromal keratitis recurs in about 10% of patients albeit in a milder form. Ghost vessels may persist for years.
References:1. Goldman J.N. and Girard KF. Intraocular treponemes in treated congenital syphilis, Arch Ophthalmol 78 (1967), pp. 47–50.
2. Smith J.L. and Israel C.W., The presence of spirochetes in late seronegative syphilis, JAMA 199 (1967), pp. 980–985
3.
Waring et al. AJO 1976