Cavernous Hemangioma of the OrbitDefinition: a benign neoplasm of the orbit characterized by congeries of large endothelial lined blood vessels separated by thick fibrous septa that contain smooth muscle.
Incidence/Prevalence: cavernous hemangioma accounts for about 5% orbital biopsies at UCLA.
Etiology: unknown but some believe that they were derived from lymphangiomas.
Clinical Findings: Cavernous hemangiomas present at a median age of about 42 years with a range between 18 and 70 in some series. There is a slight female predominance. The tumors grow slowly and are usually intraconal. With impingement on the optic nerve visual field defects such as an enlarged blind spot occur. Hyperopia may be induced by the compression of the eye. CT contrast injection fills quite slowly; separating this tumor from schwannoma, neurofibroma, hemangiopericytoma, etc.
Pathology: The gross appearance is characteristic with a nodular mass that has been likened to a cluster of grapes.
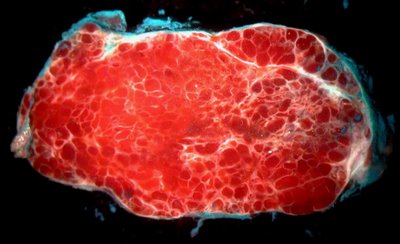
On cross section the appearance is distinctive with large (~1mm diameter) cavernous spaces filled with blood and separated by fibrous septae (white in the image). Note the green ink on the capsule of this tumor.
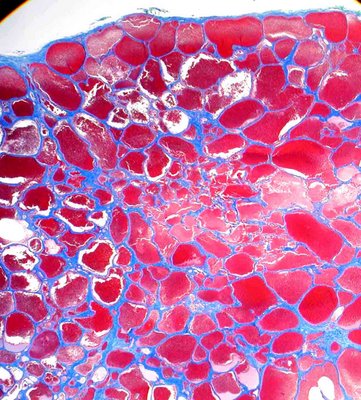
Microscopic examination shows endothelial lined channels that contain fibrous septae (blue on trichrome stain in the images). On higher magnification the septae are generally fibrous (2) but contain occasional smooth muscle cells in some areas of the wall. In the high power image the septa have been captured in an unusual tangential section that gives the appearance of a very wide septum. In this orientation smooth muscle cells are particularly obvious as they appear red in color (arrow 3) but are easily distinguished from erythrocytes in the cavernous spaces (number 1).

In longstanding cases there is often thrombosis with organization, hemorrhage and chronic inflammation.
Treatment: Excision is advocated by most, although some authors indicate that following small tumors may be adequate. The risk with surveillance is delay in diagnosis if the clinical diagnosis is in error.
Prognosis: Surgery is generally curative but the induced hyperopia and choroidal folds may persist. Deep apical lesions may present difficult in removal without injuring the optic nerve, extraocular muscles, or orbital nerves.