Definition: Noninflammatory condition characterized by the change in eye form from normal round shape to a cone shape. Cone shape results from the bilateral central or axial ectasia of the cornea with anterior protrusion of the cornea. Keratoconus results when the cornea thins and protrudes. Abnormal eye shape distorts visual images.
Incidence/Prevalence: Keratoconus usually manifest in adolescence with an incidence of about 1/2000.(
1) About 70% of cases occur in females.
Etiology: The cause of keratoconus is unknown. Keratoconus has been associated with atopic dermatitis, vernal catarrh, Down's syndrome, retinitis pigmentosa, Marfan's syndrome, aniridia, blue sclera, infantile tapetoretinal degeneration, and mitral valve prolapse. The association with atopy and vernal has led to speculation that vigorous and frequent eye rubbing may aggravate or even cause keratoconus. The cause of the central thinning is unknown but the lamellae in keratoconus are reduced in thickness, particularly deep in the stroma. A small amount of stromal thinning can be attributed to reduced number of lamellae.
Clinical Presentation: Keratoconus often manifests during the late teens or early twenties, then progresses slowly for the next decade or two as the cornea scars and becomes more elongated. Although affecting both, one eye may be more severely affected than the other. Myopia and an irregular astigmatism may result from the alteration in the normal corneal contour. Keratoconus occurs mostly as an isolated finding, but can be associated with other ocular disorders or systemic conditions (i.e. Down syndrome).
Histopathology: 
The hallmark of keratoconus is thinning of the central stroma (arrows in the lower power photomicrograph). Changes in focal disruptions of the epithelial basement membrane and Bowman’s layer are initial indicators of keratoconus.
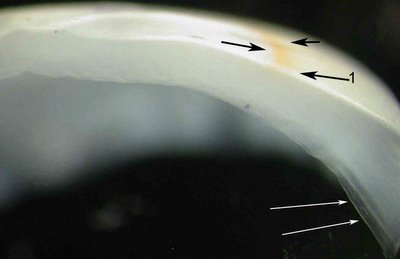
This macrophotograph of a bisected cornea is taken at the dissecting microscope with the cornea placed on edge. Here a brown ring called Fleisher's ring (black arrows) is evident on the surface of the cornea. At the very edge of the specimen (black arrow 1) the brown (oxidized iron) can be seen deposited within the epithelium. The white arrows show Descemet's membrane; click to enlarge. The central cornea (left side of photo) is thinner than the peripheral portion of the cornea.
The Prussian blue stain (Perls test) detects iron depositions in the basal epithelial layers.
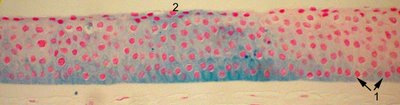
The image shows iron (blue staining at arrow 1) in the basal layer of the epithelium, which transitions to involve the entire epithelium in long standing and severe cases (arrow 2).
The earliest abnormalities of keratoconus occur in the epithelial basement membrane and Bowman's layer.
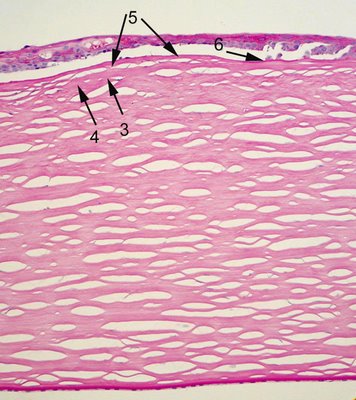
The basement membrane
may be disrupted (arrow 6) and duplicated. Bowman's layer (arrow 3) is disrupted (arrow 4) and fibrous tissue is interposed between the epithelial basement membrane and Bowman' layer (arrows 5). There is also stromal scarring. Note the endothelium is not significantly attenuated and the Descemet's membrane is thin (the patient is young).
One acute complication of keratoconus is corneal hydrops which is the sudden onset of corneal edema associated with a sudden break in Descemet's membrane. This occurs of course usually in the thinnest area of the stroma. While it can be managed medically in the acute phase, the cornea may not be able to recover as Descemet's membrane becomes scrolled and cannot heal. In this case a penetrating keratoplasty may be done.
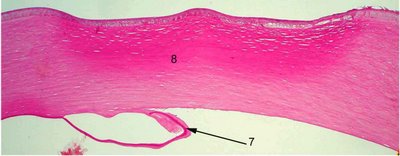
The patient whose penetrating keratoplasty specimen is shown had a history of corneal hydrops. Descemet's membrane is disrupted and folded back to rejoin the cornea in the wrong orientation (arrow 7) . There is marked stromal scarring (number 8).
Treatment: Some authors recommend cautioning patients about rubbing their eyelid as some believe this hastens progression of keratoconus. Mild cases of keratoconus can be treated with glasses or contact lenses. Often a rigid lens compensates for the irregular corneal astigmatism. Some have tried superficial keratectomy, epikeratoplasty and thermokeratoplasty with variable and often temporary improvement. Penetrating keratoplasty is considered very successful for long term rehabilitation in severe cases.