Conjunctival NevusDefinition: Acquired benign proliferation of melanocytic cells in the conjunctiva
Incidence/Prevalence: Conjunctival nevi usually appear in childhood with an increasing rate per annum. In one series the nevus accounted for about 28% of biopsied conjunctival tumors(1) . The majority of patients in some series are white but this may reflect the patient population of the series. About 2% of clinically diagnosed conjunctival nevi progressed to melanoma in one series over 7 years(2).
Etiology: unknown but the location and increasing incidence with age may suggest sun exposure is related. An activating mutation in exon 15 of the BRAF gene is associated with 40% melanomas and 50% with conjunctival nevi but not in patients with PAM (3). This work is particularly interesting as some authors claim that 1/4-1/2 of melanomas arise from pre-existing nevi (
see conjunctival melanoma in this tutorial).
Clinical Findings: The common acquired conjunctival nevus typically appears during the first decade of life. Conjunctival nevus usually (72%) develops in the bulbar conjunctiva nasally or temporally. Conjunctival nevi may also involve the plica semilunaris (11%), and the caruncle (15%). It is very unusual for limbal nevi to involve the corneal stroma, although clinically, nevi may appear to flop over onto the corneal surface. Typically the majority of nevi have cysts (65%) and about 1/3 of patients will have feeder or intrinsic vasculature. Nevi may grow, especially in children and adolescents. The sudden change in the size or color (especially towards pink or orange) in a nevus of a child or adolescent is more likely to reflect inflammation. Conjunctival melanoma is especially rare in children. Of the series reported for childhood conjunctival melanocytic lesions the incidence of melanoma was as follows:
•0/41 Bebe 1990-2001
•0/48 Goldenberg-Cohen 2005
•3/71 McDonnell 1989
•0/98 UCLA 1957-1982
One of the 3 cases in McDonnell's series developed metastases.
Age- In general the mean age of diagnosis for conjunctival nevi is younger than melanoma. In Jakobiec's recent series the mean age for nevi was 40 years of age with a range of 6-76 yrs compared to 62 yrs for melanoma with a range of 24-96 yrs. The criteria for diagnosis in this study was purely histologic and there was no meaningful patient follow up or documented history of growth.
Histopathology: 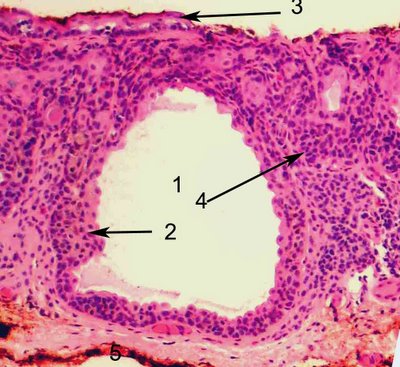
The compound nevus of the conjunctiva features nests of nevus cells that are both at the junction of the epithelium and substantia propria and within the substantia propria. The lesion is often accompanied with cystic inclusions of epithelium not nevocytes which are sometimes misleading for the neophyte. The lumen of a very large cyst (1) is shown surrounded by squamous epithelium (2). The surface epithelium has been denuded partially (3) and there are few nevus cells at the base. The nevus cells form a nesting pattern (4).
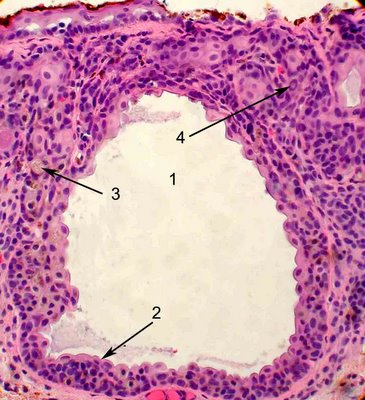
A slightly higher magnification shows the lumen of the cystic inclusion (1), the specialized stratified squamous epithelium (2), intracytoplasmic brown pigment (3) and an intranuclear cytoplasmic inclusion (4). Conjunctival nevi are believed to evolve from an initial junctional phase to a compound and finally subepithelial nevus. In the junctional phase, cells are confined to nests (theques) at the interface between the epithelium and the substantia propria. In the compound nevus phase, the nests are present in the substantia propria, as well as at the base of the epithelium and in the subepithelial phase the nests are confined to the substantia propria.
Given all of these criteria and those of immunohistochemistry, the diagnosis of conjunctival pigmented lesions remains a key problem for eye pathologists. Grossniklaus has identified discordance in diagnosis among experienced eye pathologists and has published that many melanocytic conjunctival lesions are indeterminant from the histologic findings alone.
Immunohistochemistry: Numerous studies on the immunohistochemistry of conjunctival nevi have differed in results for effectiveness. Both melanomas and nevi stain for MART-1 and S-100 and therefore have no predictive value in separating benign from malignant conjunctival lesions. Several studies have shown that HMB-45 also stains benign and malignant lesions. Two recent studies have touted that melanomas stain more intensely for HMB-45 and subepithelial nevi usually do not stain as well. These studies are all hampered by a lack of clear followup. In addition the centers reporting these studies were tertiary referral centers so that the sections had already been cut from the paraffin block and the immunohistochemistry was not performed on the same sections with the same fixation and processing. Most of the studies were not done in a stereologically sound manner. However, a recent study by
Jakobiec found that Ki-67 (a proliferation marker) did distinguish nevi (6-9% positive cells in 4 high power fields) from melanomas (19.7-34.5%). However there was at least one exception in the series of 13 melanomas. One 59 year old patient with nodular epithelial melanoma showed only 7.1% Ki-67 positive cells. There was no clinical follow up on any of these cases. The study did not address the possibility of transformation in lesions or progression. However, a panel of markers Ki-67, CD45, HMB45, MART 1 and pankeratin may be useful to 1. identify the melanocytic cells from inflammatory cells and squamous epithelium, 2. accurately gauge the depth of the lesions, 3. determine if the proliferating cells are epithelial, inflammatory or melanocytic (dual immunostaining are performed on adjacent sections).
Treatment: The treatment of pigmented lesions of the conjunctiva is predicated on an accurate diagnosis. Some lesions simply require careful surveillance. If the pigmented lesion is clinically suspicious, i.e. growth, elevation, change in pigmentation then it should be completely excised if possible. A fine (10-0) suture should be placed at 12:00 o’clock for margin analysis. Because conjunctival tissue has a tendency to curl when placed into fixative, it is important to first flatten the specimen on filter paper or cardboard face up and to float this on formalin. In this way the specimen will fix in the flat state. These lesions are best handled by eye pathologist who are used to dealing with tiny specimens for margin analysis and are quite familiar with the specific attributes of conjunctival nevi.
Prognosis: Conjunctival nevi are thought by some to be a precursor to melanoma. Shields reports that ~2% of clinically diagnosed conjunctival nevi progress to melanoma over a mean of 7 years (Shields et al. Archives Ophthalmology 2004;122:167-75). This retrospective study is based on clinical chart review that spanned a mean of 11 years and 149 patients (3 patients developed melanoma). The caveate is that the diagnosis of nevus was made clinically and there is no histologic proof that these lesions were not melanoma from the beginning. No histology was provided in the paper to document the melanoma.
References:
Shields et al. Ophthalmology 2004;111:1747-54.
Shields et al. Archives Ophthalmology 2004;122:167-75.Goldenberg-Cohen et al. Invest. Ophth. Vis. Sci 2005;46:3027-30.
JakobiecFA et al. Arch Ophthalmol. 2010;128:174-183.Grossniklaus HE et al. AJO 2000;129:702. Indeterminant melanocytic proliferations of the conjunctiva.