Primary acquired melanosis (PAM)Definition: PAM is a controversial term used to describe increased brown pigmentation of the conjunctiva, usually flat and speckled, associated histologically with an increased number of melanocytes in the epithelium. The process is acquired after birth and generally in adulthood. It has been subdivided by Folberg et al. as PAM without atypia and PAM with atypia.
Incidence/ Prevalence: There is significant difficulty in interpreting the literature about the prevalence of PAM as it is generally definition dependent. Some prominent textbooks illustrate PAM as increased pigmentation of the basal layer. In one study the prevalence of PAM was 36% in patients with no known non-European ancestry. We reserve the diagnosis for a clear increase in the number of melanocytes in a specific pattern. Otherwise patients with a dark complexion who have incidental pigmentation of the conjunctiva, benign melanosis will be included in the group. Henkind noticed conjunctival pigmentation in 92.5 % of African Americans, 28% of Hispanics and 35.7% of Asians. PAM is most common in middle-aged persons.
Etiology: unknown.
Clinical Findings: PAM presents as a speckled brown flat lesion of the conjunctiva, often a unilateral flat patch, of golden brown pigmentation with an irregular margin in a middle aged person (see photograph below).

Note in the image that the pigmentation does not diminish as one moves posteriorly from the limbus, a feature in distinction from
complexion-related melanosis. The lesions may fluctuate in size or grow slowly for 10 years or more. 46% of patients with PAM that is histologically atypical as defined by Folberg et al (see below) progress to melanoma. Patients who have PAM without atypia tend to be younger than patients who have PAM with atypia.
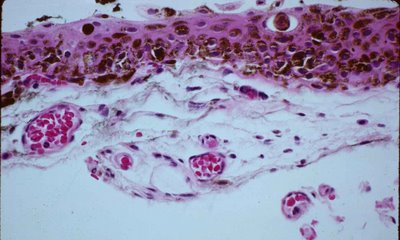
Histopathology. Histologically, PAM without atypia (Figure below) is a histologic term denoting increased pigmentation within the epithelium with hyperplasia of the basal melanocytes lacking cytologic atypia. If one uses the term, PAM, for increased pigmentation of basal epithelial cells without a proliferation of melanocytes (
benign melanosis) then entities other than our definition of PAM will be included such as
complexion related melanosis. The histologic photograph from a case of PAM shows nests of melanocytes in the basal layer of epithelium (#1 in Figure) which are poorly cohesive but confined to the epithelium. Occasional pigmented macrophages lie within the substantia propria (number 2 in Figure below).

PAM with atypia denotes atypical melanocytes which may involve or replace the epithelium with spindle or epithelioid cells. In the photograph below you see a densely pigmented lesion of conjunctiva with individual melanocytes infiltrating the epithelium. Although it is difficult to tell, the melanocyte is often surrounded by a clear space. In this case because the obvious melanocyte with a surrounding clear space is seen above the basal layer, it would meet the criteria for PAM with atypia. Of course bleaching the section would remove obfuscating pigment so cytologic atypia could be identified along with the architectural atypia that is evident here.
 Treatment:
Treatment: In general a biopsy is required for proper diagnosis of PAM. A biopsy yields prognostic information. If the lesion is small complete excision may be possible on initial biopsy and that is preferred. Extirpation has been reported with topical mitomycin; chemotherapy was found to induce regression of conjunctival melanoma and primary acquired melanosis with atypia. Cryotherapy, laser ablation, and radiation may be indicated to treat large areas of affected conjunctiva and thus spare patients the potential complications of symblepharon and dry eye associated with large conjunctiva excision. Exenteration of the orbit is not indicated for PAM, a condition that by definition is entirely intraepithelial. Often PAM exists for many years and patients undergo many biopsies.
REFERENCES- Gloor et al: Clinical characterization of primary acquired melanosis.Invest Ophthalmol Vis Sci. 1995 Jul;36(8):1721-9.
Henkind P: Conjunctival melanocytic lesion , Natual History. In Jakobeic FA Ocular and Adnexal Tumors, Birmingham, Ala, 1978 572-582.
Folberg et al. Primary acquired melanosis of the conjunctiva. Hum Pathol. 1985 Feb;16(2):129-35.
